Lasik surgery
Thanks to Miami LASIK surgery, millions of people throughout the world are less dependent on glasses or contact lenses. Still, the decision to undergo LASIK should be approached with caution. Because LASIK is still considered a surgical technique, some serious potential risks — though rare — are associated with it.
Because LASIK is an elective procedure, you should always remember that you can opt for safer and still effective nonsurgical alternatives, such as wearing glasses and contact lenses.
When considering LASIK, do some homework and consult with your eye doctor to learn more about the procedure. Ask about potential LASIK complications as well as visual outcomes.
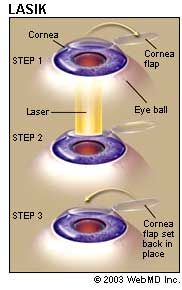
Inquire about the technology your LASIK surgeon uses for the procedure. In LASIK, an ultra-thin, hinged flap is lifted from the surface of your eye. After laser energy is applied to reshape the cornea, the flap is replaced to serve as a type of natural bandage.
Does your surgeon prefer a blade-created flap or a laser-created flap associated with the recent innovation of bladeless LASIK? You should also consider the newly developed eye-tracking technology in an excimer laser: it helps make inadvertent eye movement less of a problem during the eye surgery procedure. Also, “custom” or Wavefront-guided LASIK reduces the chance of nighttime visual side effects, such as glare and halos.
After you go through the education process to understand your best treatment options and the available technology, it is important to understand your surgeon's level of experience. After a balanced discussion about all these issues, you will be more prepared to make an informed decision, which will improve your chance of a good LASIK outcome.
LASIK Studies and Safety Standards
The eye care community sets high standards for LASIK technology. In order for a LASIK laser to receive FDA approval, manufacturers are expected to have adverse event rates of less than 1 percent during clinical trials.
The FDA definition of adverse event includes a list of specific problems such as corneal swelling, flap problems, uncontrolled intraocular pressure and detached retina syndrome.
At this time, no central database of LASIK outcomes exists. At an April 2010 public hearing, the FDA announced its intentions to clarify information about quality-of-life issues and details about what can go wrong in a LASIK procedure. The idea is to make more of these types of statistics available to the public.
Most of what is currently known about visual acuity outcomes after LASIK is based on various clinical studies, especially trials the FDA requires laser manufacturers to perform to obtain approval.
Most clinical studies of LASIK vision outcomes have a few elements in common. These include:
- An assessment of how many people achieve 20/20 vision or better (so-called "perfect" vision) and how many achieve 20/40 vision or better (the minimum visual acuity required to obtain a driver's license in most states).
- A discussion of how many people get to within one diopter or a half diopter of zero refractive error. (Myopia, hyperopia and astigmatism are all refractive errors. Zero refractive error is called emmetropia.)
- Details about possible adverse events associated with LASIK.
To monitor vision changes during the LASIK recovery period, many studies measure visual outcomes immediately after surgery, several days later and at one, three and six months after the procedure.
Comparing FDA Data on LASIK Lasers
The FDA has approved lasers for use in LASIK to treat myopia and hyperopia, with or without astigmatism. Best results have statistically occurred in people with low to moderate myopia.
When considering FDA studies, however, it is impossible to compare study results head-to-head. This is because people who enrolled in one study may have had different characteristics than those who had LASIK in another study for another company's laser.
Results from the same laser can also vary, depending on how people were selected for the study. Some studies may eliminate those with more severe refractive errors, while others may need to assess results specifically for these types of vision problems.
Furthermore, the results of studies conducted in the last few years are probably better, as surgeons gained more experience and many of the laser technologies were improved. In short, FDA results serve best to provide a general perspective of trends, but not a definitive conclusion.
Just remember that, no matter what approved treatment is best, you and your surgeon can choose to do whatever you think is appropriate and reasonable in your particular case.
Best-Corrected Vision After LASIK
The target values that the eye care community have established for LASIK vision outcomes say a lot about what you can expect from the procedure. The most feared outcome of LASIK is a decrease in best possible vision, something doctors call best corrected visual acuity (BCVA) or sometimes best spectacle-corrected visual acuity (BSCVA).
In other words, if you can be corrected to 20/20 with glasses or contact lenses before undergoing LASIK, you'd like to be corrected to at least 20/20 after LASIK.
For example, if you have 20/200 uncorrected vision before LASIK and see 20/20 with contact lenses or glasses, then see 20/40 uncorrected after LASIK but are correctable to only 20/25 with contacts or glasses, you have lost one line of BCVA (from 20/20 to 20/25) on a standard eye chart. But even though you lost one line of best corrected visual acuity, you gained more than six lines of uncorrected vision (from 20/200 to 20/40).
The FDA expects laser manufacturers to show that no more than 5 percent of patients in clinical trials lose more than two lines of BCVA and that less than 1 percent of patients have BCVA worse than 20/40.


No comments:
Post a Comment